Some people suffer from physical symptoms, such as pain or dizziness, but doctors can’t find any medical condition or physical problem that explains the cause of them. Often, some professionals and even their friends will write this off as something ‘in their head’, which can not only make the patient feel isolated but also make them question their own sanity – ‘are these symptoms really in my head?’
Fortunately, Dr Catherine Sykes, one of our top charted pshycologists, is experienced in dealing with this, which is known as medically unexplained symptoms or MUS for short. In this article, she explains how real these symptoms are, what causes them and how seeing a psychologist can help you overcome them.
What is MUS?
Psychosomatic disorders are conditions in which a person suffers from significant physical symptoms causing distress and even disability, but it is out of proportion to that which can be explained medically. These conditions are classified as MUS. Sometimes, doctors use the word functional along with other descriptions of the symptoms to categorise a MUS.
The WHO carried out a study to assess the frequency of psychosomatic symptoms across 15 countries. They found that 20% of those attending a doctor’s appointment had MUS significant enough to impact their quality of life.
Psychosomatic symptoms are influenced by the mind and can come from emotional stress, internal conflict, negative thought patterns, etc. They can also be related to behavioural issues, meaning that something that we are doing is causing physical symptoms. However, some of them are not necessarily psychosomatic, such as viral infections.
What are some classic signs of MUS?
MUS don’t obey rules. They can affect any part of the body. You can think of any physical symptom and at some time, someone’s mind and behaviours may have produced it. Examples of symptoms include:
- Fatigue
- Pain
- Visual blurring
- A loss of function such as paralysis
Is it possible that these symptoms are ‘all in my head’?
It’s important to note that the symptoms themselves are real and very distressing for the person experiencing them. I think dismissing MUS as ‘all in the head’ undermines the complexity and seriousness of the lived experience of the symptoms. This type of approach certainly does not offer any solutions and can also cause further frustration and shame that might only exacerbate the underlining cause of the MUS.
What could be possible causes?
Quite often psychosomatic disorders are due to the fact that the physical response of the organs to stress, burnout or trauma has gone too far.
How can a psychologist help someone going through a period of MUS?
A psychologist can help by understanding the experience of the person with MUS. Understanding the history of the MUS can give clues to what state of mind the person was in when the MUS started, what behaviours may be related to the origins and what behaviours might be involved in keeping the MUS going or making it worse, such as over-checking or being hypervigilant.
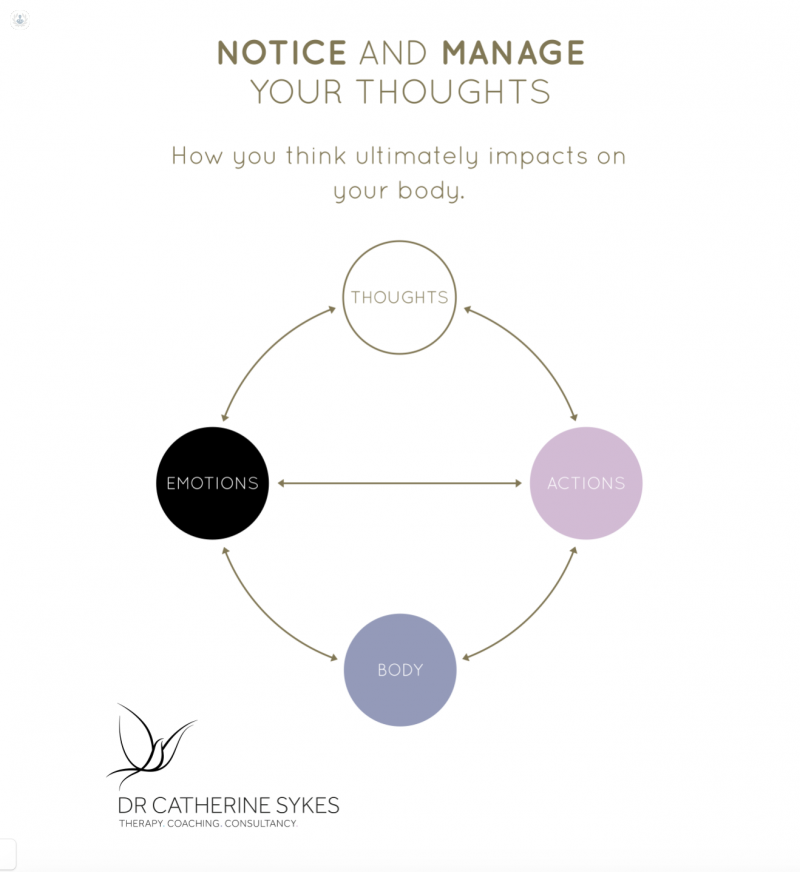
Our thoughts, emotions and everything that we do can have a significant impact on our bodies.
Psychologists can help to understand and change thinking and behavioural patterns that contribute to the MUS. They can also help clients to deal with communicating with others such as family and friends, health professionals and people in the workplace about the MUS.
Having to deal with lots of uncertainty about the MUS and the future can be very unsettling. Psychologists can help people to deal with this uncertainty and if needed, help to rethink future life goals.
